Did you know that pelvic floor physical therapist can help with constipation?
Constipation can be very complicated and for some difficult to manage, painful, and time consuming to resolve. It may take working with multiple different health care providers to help manage it including pelvic floor therapists.
What is constipation?
Constipation is when you have less then 3 bowel movements a week. Normal bowel movements are having a bowel movement 3 times a day or 3 times a week. As you can see there is a wide range of variations, and everyone is different. There can be many reasons for someone to have constipation including medication, diet, abdominal scars, medical conditions like GERD, IBS, diabetes, and Parkinson’s.
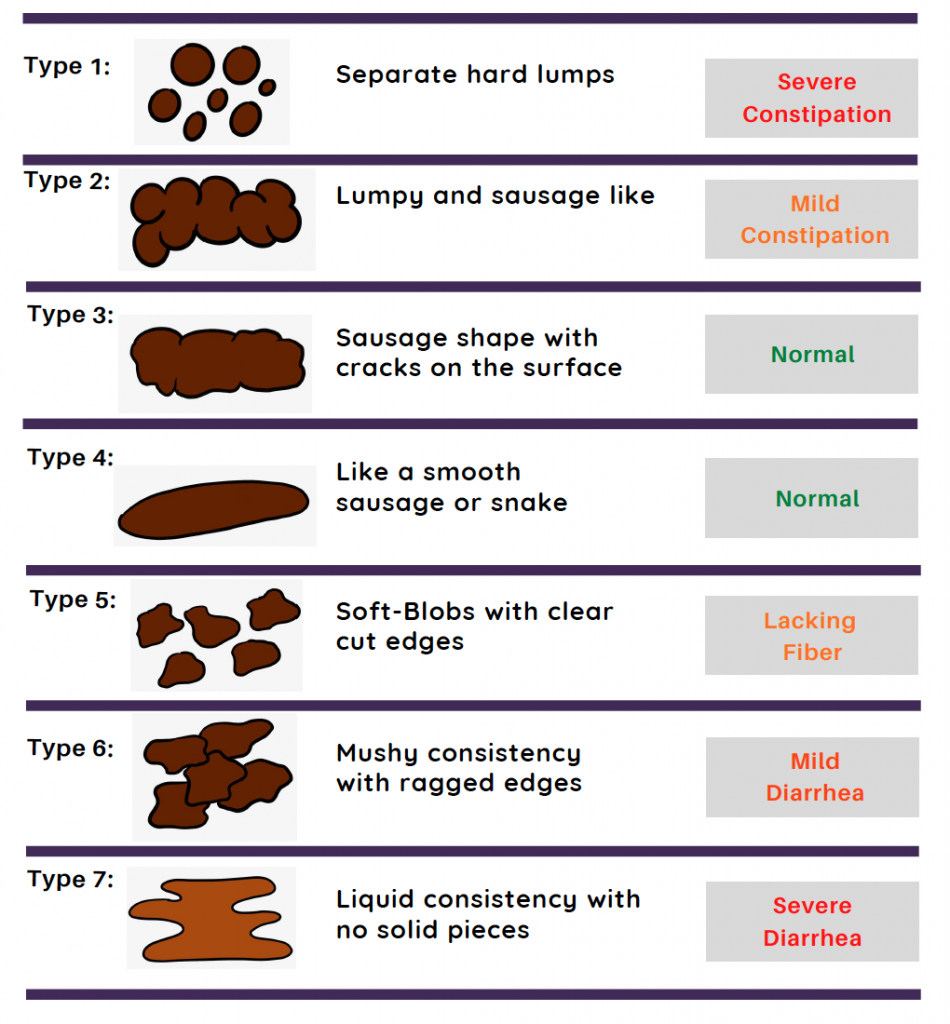
How do you tell if you have normal or “good” bowel movements?
You can look at your stool (poop) and if you are having Type 3 and 4 (banana shaped) these are considered normal. Type 4 is considered the best. If you have more types 1 and 2 then you are probably constipated. It is also possible to be constipated if you have formed stool followed by liquid stool.
What are some ways to improve bowel function?
1. Toilet training is sitting on the toilet at the same time every day and spend 5-10 minutes focusing on diaphragmatic breathing and relaxation of the pelvic floor muscle with good toilet posture (see below). It is important to not spend more than 10 minutes on the toilet and during this time you should not be straining or pushing to have a bowel movement. If you are not sure how to perform diaphragmatic breathing or pelvic floor relaxation a pelvic floor therapist can help teach you this. The time spent to empty the bowels is important it should normally only take 2-5 minutes to have a full bowel movement.
2. Relaxation of the pelvic floor muscles for some people can be difficult. A pelvic therapist can use biofeedback which will give a visual input on how you are relaxing your muscles and make sure that you are not straining to empty your bowels. It is possible to have tightness in your pelvic floor muscles that can cause you difficulty emptying bowels. Pelvic floor therapist have specialized training to help decrease tightness in these muscles using different manual therapy techniques. Just like any place else in your body that can have tightness the pelvic floor can too. Tightness in your abdomen, low back, and scars in your abdomen can also play a role in difficulty emptying bowels and your pelvic therapist can help with this.
3. Learning your body signals that you need to have a bowel movement and do not ignore the urge to have bowel movement as this can cause your brain to ignore these signals and cause you to be constipated. Make sure you are eating enough food as the rectum has pressure sensors and when there is enough weight in it will send the signal that you need to have a bowel movement. It is important that you don’t delay the urge to poop often as this will interrupt the signal to your brain. Which in the long run can add to constipation.
4. Make sure you have good toilet posture by having your knees slightly higher than your hips using a stool can be helpful to get into this position, lean forward and rest your arms on your thighs and keeping your back straight.

5. When eating you should have good posture with your feet on the floor and bring the food to your mouth. This will help line up your “pipes” so that they can function better.
6. Each bite of food should be chewed 20-40 times as this will start to help release digestive enzymes in your stomach as well as the salvia in your mouth to soften the food. Chewing your food well will also help your body with better absorption of the nutrients.
7. You should try to spend at least 20 minutes to eat your meal. Also making sure that you are eating enough food to stretch your stomach to start the gastrocolic reflex to help the digestion process.
8. Increasing your activity by even walking for 10 minutes at a time for a total of 30 minutes a day can help increase peristalsis which is the movement in your intestines to help move the food through the intestines. In the small intestines nutrition is absorbed and once it makes its way into the descending colon (last part of the large intestines) that is where the water is absorbed until the stool ends in the rectum.
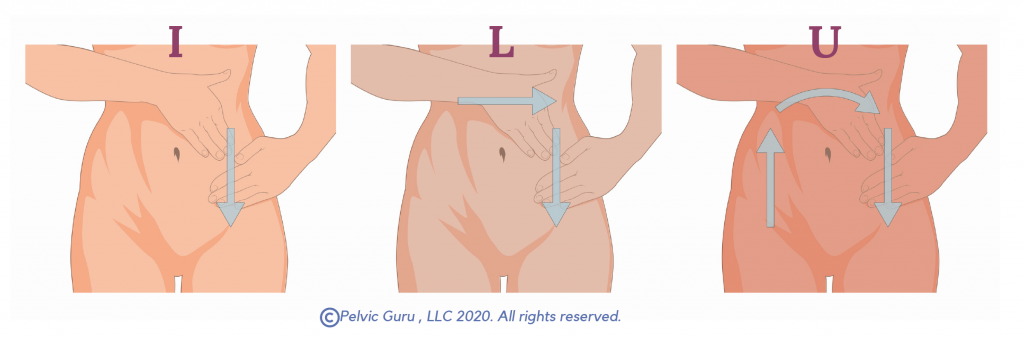
9. You can try self-abdominal massage to increase motility, decrease gas and decrease constipation. The I L U bowel massage below can be done on your own. The massage is completed with soft/light pressure.
10. You need rest to digest. Sleep is important for the digestive system and helps with maintaining your immune system. Most adults should sleep 6-8 hours to allow all 4 stages of sleep. During first 1-2 hours from when you start to sleep your body will release human growth hormone (HGH). The production of HGH and serotonin with activate peristalsis and the ability of the body to process digestion. The best time to help this is to at least get to sleep during 10pm-2am to help with HGH release and digestion.
11. Work with a nutritionist and/or your medical provider to eliminate inflammatory and common food allergies and intolerance like dairy, GOS fiber in beans, hummus and soy, Corn/Soy GMO’s. Following a FODMAP diet may also be helpful.
The digestive system takes a long time to heal and make changes. It can take 3 to 6 months with consistent modifications to have improved bowel function. With the proper tools including working with pelvic floor therapist and other health care providers constipation can be improved and with some it can be eliminated and return to normal bowel function.
Please reach out to us if you have any questions or would like to schedule a free 10-minute consult with me to see if I can help you.
*This information is for educational purposes only. Please consult with your medical provider before you make any changes to diet, exercise, medications, and supplements. *
References:
The Ultimate Bowel Course: GI and Pelvic Floor by Susan Clinton, PT, DScPT, OCS, WCS, FAAOMPT
Images used with permission from Pelvic Guru®, LLC www.pelvicglobal.com
